Breast Cancer
Breast Cancer Treatments
Videos
Your First Appointment
Diagnostic Tests
Breast Cancer Treatments
Breast Cancer Diagnosis
These days, over 90% of breast cancers are successfully treated, with an excellent long term recovery rate.
But, depending on the type and extent of your cancer, you are probably in for a bit of a rough ride over the coming months. Breast cancer treatment can have some unpleasant physical side-effects.
A cancer diagnosis and subsequent breast cancer treatment also impacts the people close to you. It can put pressure on your relationships or even cause financial hardship. You might wonder how to talk to your children, or how you are going to cope with daily living. If any of these things are a concern for you, I urge you to please talk to me. We can guide you to resources that can help with anything from household chores to financial advice.
Breast Cancer – The case for chemo before surgery
It’s perfectly understandable that when a woman finds out that she has breast cancer, her first thought is to want it taken out of her as soon as possible. But it’s not necessarily her best course of action.
Neo-Adjuvant Chemotherapy
Often it’s in the woman’s best interests to have her chemotherapy first. You may hear the approach described as neo-adjuvant chemotherapy.
The reason being that the chemo can shrink the tumours or even eradicate them. With smaller tumours, the surgeon will have a much greater chance of preserving the appearance of her breast, which is a great outcome.
It can also mean that lymph nodes might not need to be removed and lymphedema can be avoided.
With the tumour remaining in the body during chemo, the breast oncologist can clearly observe whether it is shrinking, and refine treatment according to what’s working. This fine-tuned approach to breast cancer treatment will of course also eradicate any cancer cells that may have spread from the original tumour site. And that means the risk of recurrence is reduced from X-Y%.
When the tumour is removed from the body prior to chemo, it’s impossible to have the same degree of confidence that the treatment regime is optimised for her cancer, because there is no way of observing its effectiveness.
Breast Surgery
The type of oncoplastic breast surgery I recommend to you depends on the size, extent and location of your cancer.
Where possible, I will recommend a lumpectomy, which will allow me to preserve the appearance of your breast.
If your cancer is extensive or particularly aggressive, it may be necessary to remove the whole breast. Sometimes I can do the mastectomy whilst keeping your skin and nipple for use in a subsequent reconstruction, but since sensory nerves are removed along with breast tissue, sadly sensation will be lost.
Mastectomy
If this is recommended for you, then you are going to need special care. It’s a difficult thing to have to go through, both emotionally and physically. It is hard to let go, and normal for you to grieve and take a while to come to terms with changes to your appearance.
My team and I strongly recommend that women facing mastectomy see a psychologist who specialises in breast care, to make sure that she gets the support they need to come to terms with her diagnosis, treatment and changes to her body.
It may be possible for you to have breast reconstruction surgery at the same time as your mastectomy.
Breast Reconstruction Options
There are a number of breast reconstruction options that can create a natural looking breast, which we can discuss and/or you can see one of the plastic surgeons we work closely with.
Sensation after Breast Reconstruction Surgery
Be prepared for the fact that you will have little or no sensation in your reconstructed breast, even if skin and nipple can be spared, since nerves are removed during surgery.
If the type and extent of your cancer mean that you will need radiotherapy, then my recommendation if you want to have a breast reconstruction, that you delay it until well after your treatment is finished, you need to be physically and emotionally ready.
Radiotherapy and implants
Radiotherapy is likely to compromise the quality of your skin, meaning that implants may not be an option for you. If this is your story, and you think you will want reconstruction in the future, then I can place a ’tissue-expander’ under the muscle of the chest wall at the time or your surgery. This is a ‘bag’ of air or saline, that can be expanded over time. It means that when you come to have your reconstruction, that you will have enough skin available to cover your new ‘breast’, and get a better, more natural looking result.
The downside of tissue-expanders is that they can be pretty uncomfortable for some women. I’ve heard patients complain that it’s like having a cold, hard rock in their chest, that they can only sleep on their back, that they cant run, or do high impact sport. and they even have to be careful when hugging.
Chemotherapy
Chemotherapy and radiation therapy can sometimes be given before surgery.
The technical term is neo-adjuvant treatment.We recommend it because it can shrink tumours, leading to less invasive surgery. And it means that we can monitor your tumour’s response to treatment, allowing us to tailor your therapy for your best outcomes.
Women vary in their reactions to chemotherapy drugs. It is likely that you will lose your hair, including eyelashes and eyebrows. You may also notice pigment changes on your face and nails. These are all temporary.
Chemotherapy and Changes to Your Appearance
Changes to your appearance can be distressing and may make you feel self-conscious. Our breast care nurse can book you a ‘Look-Good. Feel-Better’ workshop aimed at showing you how to cope with changes in your appearance. Read more…
Chemotherapy and side-effects
It’s really important that you tell your care team about any/all the side-effects you experience. They will ask you detailed questions before each treatment to monitor your tolerance of the drugs.
It is very common for your oncology team to recommend reducing the dosage of the medications they prescribe. Everyone responds differently to treatment, and your care team may need to tailor your medication to your specific needs. They need to find the right balance of getting rid of cancer and protecting you from unnecessary and ongoing side effects.
If they don’t specifically ask you about a symptom, then you should bring it up. For instance you may experience dry eyes, nose bleeds or pain during sex, we can help with all of these if you just let us know.
Radiation Therapy
Radiation therapy (radiotherapy) is often recommended after breast-conserving surgery or mastectomy to destroy any remaining cancer cells.
To describe why radiation is necessary after breast surgery – Here is Cancer Physical Therapy Specialist Dr. Leslie Waltke from The Recovery Room.
At your first appointment, you will be measured and x-rayed to ensure that the radiation is given precisely where it is needed. You will be given some pin-prick sized tattoos that help guide the technicians when they administer the radiation. The technician will also use a texter to make some marks on your chest.
When your regular appointments start, you will be x-rayed and measured again, and the technician will draw markings on your chest, to help guide them. The appointment will take 15minutes.
The treatments are painless, but the side-effects can include fatigue and slight skin burning at the radiation site.
To show you what to expect – here is Cancer Physical Therapy Specialist Dr. Leslie Waltke again, walking us through a radiotherapy bunker.
Hormone Blockers
Some cancers ‘feed’ off female hormones. Hormone therapy drugs ’block’ female hormones. The drugs put women into menopause, if they weren’t there already. This can cause symptoms such as hot flushes, loss of libido or painful sex.
If this happens to you, talk to Erick, he may be able to find treatment options. Don’t suffer in silence!
If you are pre-menopausal, and fertility is a concern for you, be sure to discuss your options with Erick.
Targeted Therapy
What Is Targeted Therapy?
Targeted therapies are the latest generation for the treatment of certain kinds of breast cancer. They are extremely effective, and relatively well tolerated compared to chemotherapy.
They have had a dramatic impact on survival rates for women with breast cancer. Since these drugs became available, over 90% of women have gone onto have a good long-term recovery, compared with around 75%, before these drugs became available.
They are usually be given in conjunction with chemotherapy, hormone therapy and perhaps radiotherapy.
The great thing about these drugs is that they mimic our own immune cells, attacking breast cancer cells without harming healthy cells. You may hear them referred to as mono-clonal anti-bodies, meaning that they are clones of our own antibodies that have been ‘beaten’ by HER2 positive breast cancer.
How do breast cancer targeted therapies work?
If your pathology results show that you have HER2 positive breast cancer, it means that your cancer cells are carrying too many receptors for an abnormal protein called HER2 on their surface.
When the HER2 receptor is activated, it stimulates the growth of breast cancer cells. Targeted therapy uses drugs that attach to these receptors to inhibit or stop their action. It acts a bit like a lock and key. The drug ‘locks’ onto the receptor, creating a barrier that stops the HER2 from connecting to it.
This locking also tags the cancer cell helping your immune system to recognize and destroy it.
Women with HER2+ cancer may be recommended treatment with drugs such as, Trastuzumab (Herceptin®), Pertuzumab or lapatinib (TYKERB®).
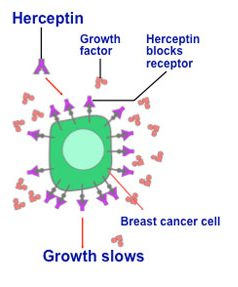
It may be given alone or with chemotherapy. Most women have minimal side effects from Herceptin, but it’s possible that you may experience fever and chills during the first treatment.
A known side effect of Herceptin is that can cause fluid to gather round your heart. So your oncologist will make sure that your heart is checked before during and after treatment. It is very important that you tell your oncologist if you find yourself getting breathless or are unable to do your normal activities.
Some chemotherapy drugs can also be hard on your heart. If these drugs are recommended for you, then your oncologist will not give you Herceptin at the same time as the chemotherapy drug.





For all appointments and enquiries, please call +61 2 8203 1359 or email info@drerickfuentes.com.au
Or contact us online using this form:
Request an Appointment Or Send a Message
Wise Medical
Level 1
11 Khartoum Road
Macquarie Park
NSW 2113
Strathfield Private Hospital
3 Everton Rd,
Strathfield NSW 2135
Hours: 9am - 5pm
Follow Us
© 2023 Dr Erick Fuentes. Breast and Endocrine Surgeon.